Children’s Eye Examinations: When and How to Check Your Child’s Vision
12/01/2026
03/07/2025
Do you know you can have glaucoma without high eye pressure?
Low-tension glaucoma, also known as normal-tension glaucoma (NTG), is a condition in which damage to the optic nerve characteristic of glaucoma occurs, with visual field defects also characteristic of glaucoma (scotoma) , but with intraocular pressure (IOP) is within the normal range (10-20 mmHg).
The great impact of this disease is that when it is diagnosed, there is already irreversible damage to the optic nerve, since it cannot be predicted in any other way, so in these patients, an adequate diagnosis and treatment according to their situation are crucial.
The exact cause of this glaucoma remains unknown, but what is known is that in many cases there is an underlying systemic vascular problem, such as sleep apnea syndrome, severe anemia, Raynaud's syndrome or severe nocturnal low blood pressure…In the case of normotensive glaucoma, a detailed study must be performed to rule out these underlying pathologies as well as masquerade other neuropathies that can produce changes in the optic nerve that simulate glaucoma and they should be taken to investigate adequately.
Despite IOP remain within normal limits range, there is evidence that an IOP-dependent mechanism plays a role in the etiology of the NTG, and that is why management includes reducing IOP, as occurs with glaucoma with high IOP.
Risk factors related to NTG are age, family history, there are 3 gens related to this condition Optineurin (OPTN), TANK binding kinase (TBK1), Myocilin (MYOC), females gender, thin cornea thickness, systemic hypertension above all with nocturnal hypotension, migraine, Raynoud phenomenon, frontotemporal and Alzheimer dementia and obstructive sleep apnea.
Patients are usually asymptomatic at presentation, with suspicion of glaucoma raised by an ophthalmologist on routine eye testing or an incidental finding. Even with moderately advanced disease, patients may be unaware of field defects because of unilateral disease, negative scotoma, and gradual onset. Because the IOP is normal, suspicion is usually roused by optic disc appearance or a visual field defect on automated perimetry. If the presentation is advanced, patients may have symptoms of reduced vision, difficulty with low-contrast situations, and awareness of visual field defects. They may experience glare and difficulty adjusting to extreme lighting conditions. A family history of glaucoma and blindness should be obtained. Past medical history should include assessing risk factors for glaucoma, such as the history of steroid use, ocular trauma or surgery, and contraindications to treatments, including allergies. Medication usage should be reviewed.
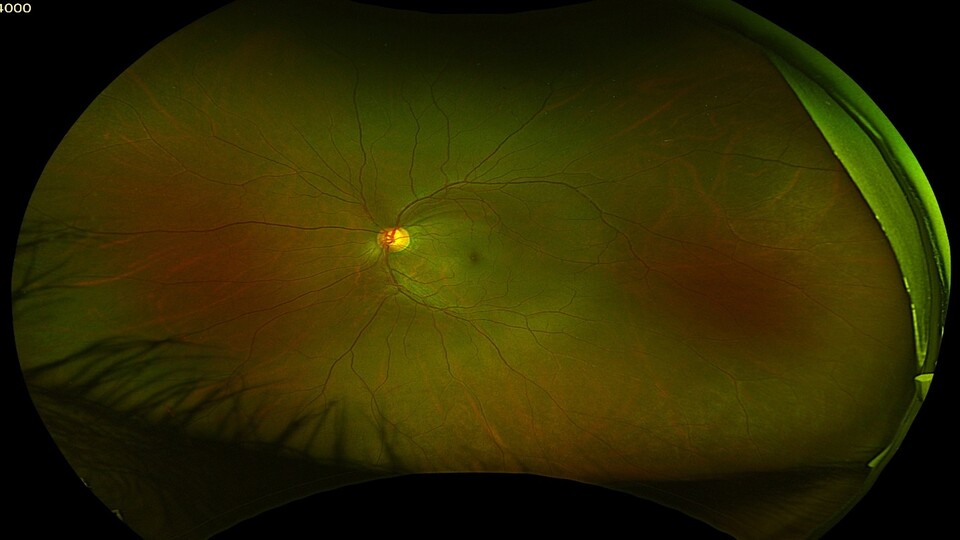
Slit-lamp examination and gonioscopy are essential to determine an open iridocorneal angle status and exclude secondary glaucoma causes. In particular, evidence of angle closure, uveitis, pigment dispersion, and pseudoexfoliation syndrome should be sought, as these are common causes of glaucoma presenting with an IOP in the normal range. A dilated fundus examination revealed changes in the glaucomatous optic disc. There is a progressive loss of ganglion cell neurons, leading to enlargement of the cup-to-disc ratio. This may be a focal (notch, retinal nerve fiber layer (RNFL) defect) or concentric defect (excavation, senile sclerotic disc). Disc pallor occurs in advanced disease. Measurement of the optic disc size can help identify hypoplasia, physiological disc cupping, and disc asymmetry. Optic disc hemorrhages are more common in NTG than in POAG. So-called Drance hemorrhages are typically small flame hemorrhages at the disc margin in superior or inferior quadrants. Peripapillary atrophy may be seen but is non-specific. Glaucomatous disc abnormalities typically precede visual field defects in early (preperimetric) disease.
The treatment includes the decreasing of the IOP despite being within normal ranges with topical medications, laser, or surgery in the same way we would do with open-angle glaucoma with high ocular tension but in NTG we should considered the treatment of the risk factors associated as nocturnal hypotension , is mandatory a 24-hour blood pressure analysis and avoiding nighttime dosing systemic anti-hypertensives. Diet and nutritional supplementation with Nicotinamide (vitamin B3) and ginkgo biloba but it still under investigation can be useful. Rule out and treat accordingly the sleep apnea syndrome. Regular exercise is associated with lower IOP afterward, but a positive or negative effect on the pathogenesis of NTG is unknown. Exercise is beneficial for many other aspects of health and should not be discouraged. However, yoga positions held for extended periods that position the eye below the rest of the body (such as headstands or downward dog) can significantly raise intraocular pressure, and case studies have shown rapidly progressive disease. Other practices such as meditation could lower IOP, reduce IOP fluctuation, and positively affect neuroprotective markers. And avoid smoking, it may be associated with both raised IOP and glaucoma.
Glaucoma is the second most common cause of irreversible blindness worldwide and is a public health concern in both the developed and developing world. Early detection is challenging due to the lack of symptoms. Educating the public on the importance of regular eye exams facilitates the detection of NTG and other eye diseases. Patients who are diagnosed with glaucoma should be instructed to advise first-degree relatives to have regular eye exams to enable early detection.
For consultation, please contact us:
Our team will be pleased to assist you.