Could Age related Macular Degeneration be prevented?
15/02/2022
Age-related macular degeneration (AMD) is a degenerative disease of the macula that causes gradual loss of central vision. The macula is a small area located in the centre of the retina, the posterior layer of the eye that transforms the light and images that enter the eye into nerve signals that are sent to the brain.
The macula is responsible for helping us see little details clearly, for our vision being as sharp up close as it is at a distance. AMD only affects central vision, it does not change our peripheral vision.
It is the most common cause of a severe loss of vision in the Western world. In Spain, it affects 13% of people over 65.
In addition, as it is closely linked to ageing, it is estimated that the number of people with macular degeneration could double in the next 20 years due to the increase in the life expectancy of the population.
We can classify AMD into 2 variants, with different evolutions and prognoses:
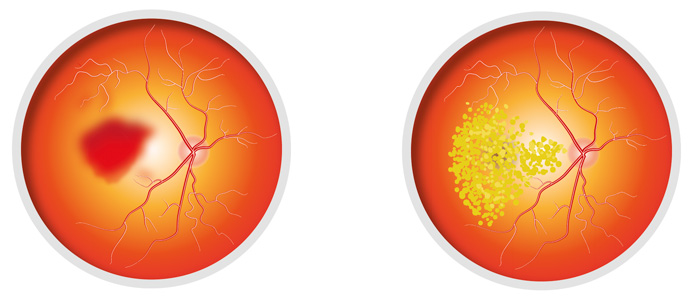
On the left: wet or exudative AMD. Diagram on right: dry or atrophic AMD.
In the most mild cases and when only one eye is affected, patients may not have symptoms. However, when the disease progresses, the patient may suffer from some of the following symptoms:
The foregoing will lead to difficulty performing daily tasks like reading, writing, driving, cooking, etc. If you have any alarming symptoms, you should see an ophthalmologist to undergo an assessment and be treated as quickly as possible, thereby limiting the irreversible visual sequelae that cause AMD.
As it is a disease inherent to ageing, there is no prevention, although early diagnosis and treatment will mean a better visual prognosis.
It is advisable to undergo regular eye check-ups from the age of 50, especially if you have a medical history. And if there is any change in your eyesight, please see an ophthalmologist without delay.
Before starting any treatment, you must undergo a full eye examination. On occasions, we undertake a fluoroscein angiography (the injection of an endovenous contrast dye that helps us to study the location and size of the neovascular membrane in greater detail) to confirm the diagnosis and an optical coherence tomography (a scan of the macular to that shows indirect signs of the disease's activity) to help us during follow-up.
Wet or exudative AMD must be treated with intravitreal injections of antiangiogenic drug (Ranibizumab, Aflibercept or in selected cases, Bevacizumab). This has helped us to delay or even stop the progression of the disease in a large number of patients. Currently, 70% of patients treatment manage not to lose their eyesight and 40% end up having eyesight above 0.5, which means it is possible for them to drive.
For greater safety and the comfort of the patient, intravitreal injections should be administered in the operating theatre or a clean room, and therefore, under strictly sterile conditions. Their administration is practically painless, as anaesthetic drops are put in the eyes and it is well tolerated by patients. It does not require a pre-operative period. The post-operative period only requires the use of antibiotic eyedrops to prevent infections. The risk of complications is extremely low if these guidelines are followed.
There is still no cure for atrophic AMD. Taking antioxidant complexes, eating a healthy diet (rich in antioxidants and Omega 3), avoiding smoking and limiting sun exposure, seem to slow the evolution of the disease.